Eckardt Johanning,1 Paul Landsbergis,2 Manfred Gareis,3 Chin S. Yang,4 and Ed Olmsted5
1Mount Sinai School of Medicine, New York, New York USA; Eastern New York Occupational and Environmental Health Center, Albany, New York USA; 2Cornell University Medical College, Mount Sinai School of Medicine, New York, New York USA; 3Federal Meat Research, Microbiology and Toxicology, Kulmbach, Germany; 4P&K Microbiology Services, Inc., Cherry Hill, New Jersey USA; 5Olmsted Environmental Services, Inc., Garrison, New York USA
Methods
Study Group Selection and
Description
This is a descriptive study of patients evaluated in an ambulatory
occupational and environmental health clinic, including self- and
physician-referred patients primarily from the northeastern United States. A
sample of patients less than 18 years of age was selected as a pediatric
sample because at that age completion of major organs and lymphoid maturity
are achieved. The pediatric sample (age < 18 years, n = 22; mean age
9 years; 60% females) and a sample of adult patients (age >18 years, n
= 125; mean age 39 years, 67% females) were included if they had a
verifiable history of indoor exposure to fungal air contaminants and if they
had completed a standardized health symptom questionnaire. Fungal exposure
was considered positive if industrial hygiene survey information and data
confirmed the presence of fungi and significant moisture problems (leaks,
flooding, condensation, etc.). In addition, for comparison, descriptive data
from an earlier study are presented that included well-documented exposure
and that used the same core questionnaire. The earlier study included a
nonexposed adult population with similar demographics as a control group (11).
Health Symptoms Survey
The health symptoms survey had been adapted with slight modification from
the Mount Sinai Medical Center Fungal Health Survey Questionnaire (11).
Cumulative symptom complex scores were computed by combining separate
questions related to particular organs: upper respiratory system (nasal
irritation, burning, itchiness, stuffiness and congestion, nasal bloody
discharge, throat irritations, and soreness); lower respiratory system
(cough, shortness of breath, wheezing, chest congestion, and tightness);
central nervous system (severe headaches, concentration problems,
irritability, dizziness or lightheadedness, sleeping problems, fatigue);
eyes (burning, irritation, blurry vision); skin (burning, erythematous rash,
hair loss); constitutional (low-grade fever, tender/swollen lymph nodes,
flulike symptoms), and history of previously diagnosed allergy.
Laboratory Testing
Laboratory tests were performed to study red and white blood cells,
multichemistry, and immunological parameters. The medical laboratory tests
were analyzed by licensed commercial labs following standard quality
assurance procedures (IBT Laboratory, Kansas, MO; Specialty Laboratory,
Inc., Santa Monica, CA). To evaluate possible type I allergic reactivity,
allergen-specific IgE was tested in a panel for Cheatomium globosum;
Aspergillus fumigatus; Cladosporium; Penicillium notatum; S. atra;
mouse, rat, and pigeon serum proteins; and American cockroach. A panel of
IgG was measured and considered as marker of exposure for Micropolyspora
faeni, Thermoactinomyces spp., Alternaria alternata, A. fumigatus,
Aureobasidium pullulans, P. notatum, Phoma herbarum, Trichoderma viride,
pigeon droppings, pigeon serum, bovine serum, Cladosporium, and S.
atra. Allergen testing material was provided by Pharmacia & Upjohn
Diagnostics (Bridgewater, NJ).
Exposure Assessment
Indoor exposure to fungal materials was assessed and verified by experts in
the field generally relying on test methods described by the American
Industrial Hygiene Association field guide for the determination of biologic
contaminants (18). Indoor exposure was characterized using
microscopic, culture, and mycotoxin cytotoxicity screening tests (MTT).
Subjects with a history of indoor fungal exposure that was deemed to be
excessive or atypical compared to outside or other references were included
in the analysis presented here.
Sentinel Case Example
In addition to the epidemiologic data, a clinical case example is presented
here to illustrate the complexity of comprehensive exposure and health
assessment and also to document the benefits of a positive environmental
intervention outcome (exposure cessation). In the case investigation, the
indoor environment and health complaints of a low-income family living in an
apartment building in Spanish Harlem, New York, were examined. The apartment
had a longstanding history of moisture problems and widespread visible
fungal growth on interior surfaces (> 100 ft2). The mother of an
eleven-year-old daughter had noticed that the general health of her daughter
improved when she was away from the New York apartment. The daughter had a
history of recurrent bouts of asthma, pneumonia, bronchitis, sinusitis, and
middle ear disease. Upon return to the apartment, previous symptoms and
illnesses recurred or worsened. Observations by the primary care providers
confirmed this history. It should be noted that the daughter (index
case/subject A) had a diagnosis of velo-cardio-facial syndrome (a variant of
DiGeorge syndrome), which is associated with T-cell deficits due to thymic
hypoplasia and an increased susceptibility to infections. Although this
condition is associated with disorders similar to or identical with the
studied fungal outcomes, this case was chosen nonetheless because the
history of symptoms given by the mother suggested that environmental factors
strongly influenced the girl's health. Other family members were also
included in the case study, as they also reported variation of their health
status dependent upon environmental changes. A suitable case control was not
available and such a study was not feasible at the time of this
investigation. However, the adult occupant of the apartment that was used as
a control in the environmental assessment was asymptomatic and free of any
atopic diseases.
We investigated the environmental conditions inside the apartment and compared them to outside conditions and a reference apartment inside the same building that did not have visible evidence of moisture and fungal problems (healthy adult occupant). In addition to the index case, the brother (subject B; 21 years of age) and the mother (subject C; 50 years of age) were studied because they reported symptoms, although less severe. Subject A (who had lived since birth in the apartment) and subject C spent most of a typical day inside, whereas subject B was only in the apartment during the night. The family was removed from the contaminated apartment and retested after a period of 8 weeks (pulmonary function and T-lymphocyte flow cytometry) and again after 4 months (lymphocyte flow cytometry). There were never any pets in the apartment. The apartment building had a known history of cockroach and rat infestation.
Fungal Exposure Sampling
Viable fungal air samples were collected on cornmeal agar and malt extract
agar using a single-stage (N6) impacter (Andersen Instruments Inc., Atlanta,
GA) operated at a flow rate of 28.3 L/min for 2 min. Total airborne fungal
materials (including nonviable spores) were sampled using an Arca sampling
pump and Air-O-Cell air sampling cassettes (SKC, Inc., Eighty Four, PA) with
a 15 L/min flow rate for 3 min. The cassettes were analyzed; results were
reported in fungal structures per cubic meter of air.
Toxicity Screening
The MTT cytotoxicity screening test is particularly sensitive to S.
chartarum toxins (i.e., Satratoxin). The MTT cell culture assay and a
swine kidney target cell line were used as a direct method. Bulk samples
were tested directly in the toxicity tests for presence of mycotoxins (19,20).
The principle of this bioassay is based on the transformation of the yellow
tetrazolium salt MTT by viable, living cells (via mitochondrial
dehydrogenase) to purple formazans. The optical density of the formazans can
be measured by an enzyme-linked immunosorbent assay (ELISA) reader at a
wavelength of 540 nm. Swine kidney monolayer cells (SK), known to be
sensitive to mycotoxins, were used as target cells. The minimum
concentrations of the test reagents to cause toxic effects were determined
on the basis of the statistically determined values of 80% cleavage
activity.
Cockroach Antigen Sampling
Dust samples were collected using filter media attached to a vacuum cleaner
hose. Approximately 1 m2 of floor surface was vacuumed. The dust
samples were analyzed using an immunologic assay to identify the presence of
a cockroach allergen (Bla g 1). Results are reported in micrograms of
cockroach allergen per gram of dust (ĩg/g).
Pesticide Sampling
A 100-cm2 area of floor surface was wiped with sterile gauze
saturated with toluene. The sample wipes and bottles were prepared, and
later all samples were scanned by the Wisconsin Occupational Health
Laboratory (Madison, WI) for presence of pesticide contamination.
Dust mite or other animal antigens were not measured. (This was a winter period and no household animals were present.) Other chemical or organic compounds were not measured because the industrial hygienist did not observe any unusual presence or use of household chemicals. An indoor asbestos and lead screening was negative.
Results
Review of Clinic Records
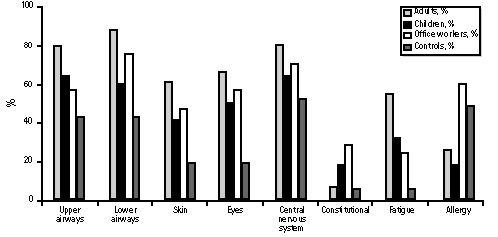
The analysis of clinically recorded health symptoms and organ complaints of patients with a history of indoor fungal exposures showed a high prevalence (> 50% of all respondents) of symptoms of upper and lower airways, eyes, and central nervous system. Children also showed a high prevalence of symptoms, although the absolute percentage rate was slightly lower than that of adults (Table 1, Figure 1). Compared to the office workers with health problems associated with fungal exposure and the nonexposed controls, children appeared to complain slightly more about upper airway problems (symptoms related to rhinitis, sinusitis, laryngitis) and slightly less about lower airway problems (symptoms related to bronchitis, asthma, or pneumonitis). Skin, eye, and central nervous system complaints were present in more than 40% of respondents, with similar high proportions for the adults. Excessive physical and mental fatigue (fatigue) was reported by about one-third of the children interviewed and by about half the adults (54%). The rate of preexisting and diagnosed allergy in patients was less than 20% and lower than in the comparison groups. The higher prevalence of symptoms among patients and exposed office workers relative to nonexposed controls was not likely due to group differences in age, gender, or smoking, as groups were similar on these potential confounders (except, of course, for the younger ages of children).
Figure 1. Health survey: children vs. adults. For explanation of office workers and controls, see text.
Five percent of the children had any evidence of specific IgE antibodies to tested fungal allergens (except S. atra), 9% had an IgE reaction (borderline values), and none had an elevated IgG (> 40 mcg/mL) to S. atra. None of these children had a specific antibody reaction to cockroaches. Complete lymphocyte and other immunoglobulin analysis were available for only five children and are not reported here. On the basis of the review of available industrial hygiene data, about 90% of the children had verifiable exposure to higher-than-normal indoor levels of primarily Penicillium and Aspergillus spp., and at least 41% of the children had documented exposure to S. atra.
Sentinel Case Example
Results of the clinical evaluation showed that all three subjects had
objective evidence of respiratory disorders (mixed restrictive and
obstructive abnormalities) and abnormalities of the T-cell flow cytometry
subgroups (Tables 2, 3). Subjects A and B had very low CD4 counts, although
no histories of HIV infection or similar risk factor for low CD4 T-cell
counts were evident except for the verified genetic defect (velo-cardio-facial
syndrome) in the index case. The ratios of CD4/CD8 were low and remained low
after removal (1.2-1.4) in all subjects. Subject A had a low positive
elevation of IgE to S. atra (873 counts) with a borderline total IgE
elevation of 138 (> 158 indicative of atopic allergy). Subject B had no IgE
or IgG elevation. None of the subjects was allergic to cockroach allergen.
After leaving the apartment, all subjects reported a marked improvement and a partial resolution of their health problems. Less frequent and severe cough episodes, less chest discomfort, and fewer breathing problems, headaches, fatigue, and flulike symptoms were noted. Pulmonary function improved in all three subjects (Table 2) and the lymphocyte enumeration measured 8 and 16 weeks after removal (Table 3) appeared to show some minimal improvement in some parameters. The index case had a PWM and CON mitogen response abnormality during the exposure period (data not shown). The results of the T-lymphocyte function (mitogen proliferation) tests performed 16 weeks after removal were normal in all subjects. These results and the lack of clinically significant viral or bacterial infections after removal from exposure indicate only a minor remaining immunodeficiency, which could be explained by the known preexisting genetic abnormality.
Inside the apartment, approximately 70-100
m2 of surface area (walls, ceilings, around the window air
conditioning unit, the doors, and window frames) were covered with a
blackish-colored growth. Airborne fungal counts (viable and nonviable) were
significantly higher (10-200 ![]() ) than the
outside or the control apartment used as a reference (Table 4). Predominant
indoor airborne fungi were Cladosporium, Aspergillus, Penicillium,
and S. chartarum. Bulk samples taken from the problem apartment
showed a high concentration of S. chartarum, A. versicolor, and
Cladosporium. All bulk samples taken from the home (bedroom, bath, and
kitchen) were toxic to highly toxic in the MTT screening test.
) than the
outside or the control apartment used as a reference (Table 4). Predominant
indoor airborne fungi were Cladosporium, Aspergillus, Penicillium,
and S. chartarum. Bulk samples taken from the problem apartment
showed a high concentration of S. chartarum, A. versicolor, and
Cladosporium. All bulk samples taken from the home (bedroom, bath, and
kitchen) were toxic to highly toxic in the MTT screening test.
Cockroach allergen Bla g 1 in sampled floor dust was considered high, based on the classification by the National Cooperative Inner-City Asthma Study, although the maximum concentration in the Inner-City Asthma Study was 1,190 U/g dust [median 8 U/g) (21)]. No pesticide toxins were detected inside the apartment.
Discussion
The symptom survey of children evaluated in our specialty clinic indicates a high rate of morbidity related primarily to the upper airways, skin and mucous membranes and, to a lesser degree, lower airways. In all cases we confirmed that these children had all been living in indoor environments with high levels of fungi, often species not normally found indoors or in such concentrations compared to the outside air (i.e., S. chartarum, A. versicolor, Trichoderma). Our results are in agreement with a number of previous studies. A recent review of the literature investigating the association of wheeze and cough and damp or mold found that the adjusted odds ratio for an increased risk of children was generally in the range of 1.5-3.5 (22). The high rate (about two-thirds) of central nervous system problems among children from moldy homes suggests a complex exposure-associated morbidity reaction with a pathologic pathway that cannot readily be explained by atopy or allergy (IgE-mediated). The health complaints summarized by organ system were similar for children compared to adults, although the absolute percentage rate of complaints was slightly lower for children. The rate of reported symptoms was higher than that of a nonexposed adult control group in almost all categories except for a previous diagnosed history of allergy. None of the queried children had evidence of an allergy to cockroaches, which has been described as an important predictor of environmental-associated asthma (21). On the basis of our assessment of the clinical cases, morbidity related in time and place to indoor fungal exposure appears to be widespread in environments with a history of flooding, water leaks, moisture problems, and ventilation defects that resulted in intense fungal growth on interior building materials or furniture.
Differences were not analyzed for statistical significance because of methodological issues and limitations such as small sample size and different time and location of measurements. The response variations and group differences may be due to selection bias, biologic differences, or survey limitations (e.g., children were less used to questionnaire formats, were unfamiliar with interview techniques, or were assisted by parents).
Only 2 children and 13 adults had positive (abnormal) laboratory findings for the presence of IgE- and IgG-specific fungal antigens. In this small sample, neither the presence of positive antigen findings nor a fungal exposure history showed a statistically significant association with symptoms. The small number of subjects with abnormal laboratory findings (only 5 children had undergone complete lymphocyte testing) did limit the statistical power of analysis of group differences in laboratory findings. The differences in laboratory test results may be related to a variety of factors including the differences in exposure duration, latency, timing of laboratory testing relative to exposure and testing, and temporary medical treatment effects. A study of a larger number of children with similar exposure (children in kindergarten or schools) that included testing of biologic markers at the same time would be beneficial for epidemiologic studies. Presently there is not a reliable mycotoxin biomarker available for clinical screening studies. Therefore, clinicians rely on indirect laboratory effects measures such as T-lymphocyte responses and immunoglobulins counts. Advances in immunology, laboratory, and diagnostic methods may ease clinical diagnosis in the future.
In the case example investigation, a key factor was the reported history of variability of health complications depending on the indoor environment, i.e., the dramatic health improvement away from the fungal exposure inside the apartment. We presented this case example because it appears to demonstrate that such fungal exposure can significantly aggravate and complicate pre-existing immunological disease. The exposure was not only affecting the index case but also the brother and mother who shared the apartment with her but had no history of genetic abnormalities. Inside the apartment we identified very high levels of fungi indoors, with a predominance of Cladosporium and toxigenic S. chartarum. The presence of airborne S. chartarum in indoor environments is considered by experts to be highly uncommon in normal buildings and unacceptable from a public health perspective. The MTT cytotoxicity tests showed that all samples taken from the girl's home environment had toxic metabolites (such as trichothecene) in the fungal materials. The fungal mass (spores) would have become airborne when disturbed.
Blood lymphocyte changes effecting the T-lymphocyte differentiation and subpopulation proportion were measured as in previous studies (11,23). Changes of the T-lymphocyte population were demonstrated in in vitro and in vivo studies but remain difficult to interpret on an epidemiological level because of only very small differences and variations in observed trends. In our case example, some lymphocyte parameters showed improvement after exposure cessation, but these may be within laboratory and normal daily variations. Only the index case had genetic evidence of a deletion of 22q11.2, confirming a velo-cardio-facial syndrome (DiGeorge variant). Cockroach antigen (Bla g1) exposure, although present in high concentration, did not result in measurable allergies in any of the apartment occupants. On the basis of available data and the observed health improvement with exposure cessation, we concluded that indoor fungal exposure was the probable contributing cause of the health problems associated with living in this apartment. Some other unidentified agents or conditions may have also contributed to the improved outcome, although we think this is very unlikely under the circumstances. Studies of health outcomes related to bioaerosol exposure appear more complicated than monoagent chemical exposure studies because several biologic components (i.e., ß-glucans, microbial volatile organic compounds, endotoxins, allergen, mycotoxins) may have independent or combined effects.
It is our clinical experience that symptoms associated with mold exposure tend to resolve with exposure avoidance and symptomatic treatment. In some individuals, symptoms may last several weeks to months after exposure control and in some rare cases may not be reversible at all. A highly increased sensitivity with recurrent fungal exposure has been noted by some individuals. These variations in the postexposure periods may be related to differences in the exposure duration, intensity, and particular conditions (different fungal species), the biologic differences of the immune reaction of exposed individuals, and the type of medical intervention or treatment.
Children with preexisting, significant immunological weaknesses and defects are at increased risk and should be protected from unnecessary fungal exposure. Long-term benefits of such intervention (secondary prevention) and related health indicators should be studied more systematically. Fungal exposure in indoor environments should be included in future environmental respiratory and immunologic disease studies, in addition to already known indoor pollutants. It is necessary for the physician examining a child with complex respiratory problems, allergy, nervous system disorders, and perhaps other organ system problems, to inquire about problems in the home such as chronic water leaks, extensive interior condensation, flooding, and especially visible fungal growth on interior building materials. In many cases, effective fungal exposure control and avoidance may be all that is needed to achieve a significant improvement in the child's health.
REFERENCES AND NOTES
1. Husman T. Health effects of indoor-air microorganism. Scand J Work Environ Health 22:5-13 (1996).
2. Reijula K. Building with moisture problems--a new challenge to occupational health care. Scand J Work Environ Health 22:1-3 (1996).
3. Hintikka E-L. Human stachybotryotoxicosis. In: Mycotoxic Fungi, Mycotoxins, Mycotoxicoses, Vol 3 (Wyllie TD, Morehouse LG, eds). New York:Marcel Dekker, 1978;87.
4. Croft WA, Jarvis BB, Yatawara CS. Airborne outbreak of trichothecene toxicosis. Atmos Environ 20:549-552 (1986).
5. Mainville C, Auger PL, Smoagiewica W, Necukcea D, Neculcea J, Levesqye M. Mycotoxins and chronic fatigue syndrome in a hospital. In: Healthy Buildings Conference (Andersson K, ed). Stockholm:Swedish Council of Building Research, 1988;1-10.
6. Auger PL, Gourdeau P, Miller JD. Clinical experience with patients suffering from a chronic fatigue-like syndrome and repeated upper respiratory infections in relation to airborne molds. Am J Ind Med 25(1):41-42 (1994).
7. Johanning E, Auger PL, Reijula K. Building-related illnesses. N Engl J Med 338(15):1070 (1998).
8. Montaņa E, Etzel RA, Allan T, Horgan TE, Dearborn DG. Environmental risk factors associated with pediatric idiopathic pulmonary hemorrhage and hemosiderosis in a Cleveland Community. Pediatrics 99(1):1-8 (1997).
9. Sorenson B, Kullman G, Hintz P. NIOSH Health Hazard Evaluation Report. HETA 95-0160-2571. Morgantown, WV:Centers for Disease Control and Prevention, 1996.
10. Etzel RA, Montaņa E, Sorenson WG, Kullman GJ, Allan TM, Dearborn DG. Acute pulmonary hemorrhage in infants associated with exposure to Stachybotrys atra and other fungi. Arch Pediatr Adolesc Med 152:757-62 (1998).
11. Johanning E, Biagini R, Hull D, Morey P, Jarvis B, Landbergis P. Health and immunology study following exposure to toxigenic fungi (Stachybotrys atra) in a water-damaged office environment. Int Arch Occup Environ Health 68(4):207-218 (1996).
12. Johanning E. Stachybotrys revisited. Clin Toxicol 36(6):629-631 (1998).
13. Hodgson MJ, Morey P, Leung WY, Morrow L, Jarvis BB, Robbins H, Halsey JF, Storey E. Building-associated pulmonary disease from exposure to Stachybotrys chartarum and Aspergillus versicolor. J Occup Environ Med 40(3):241-249 (1998).
14. Corrier DE. Mycotoxicosis: mechanism of immunosuppression. Vet Immunopathol 30:73-87 (1991).
15. Sharma RP. Immunotoxic effects of mycotoxins. In: Mycotoxins and Phytoalexins (Sharma RP, Salunkhe DK, eds). Boca Raton, FL:CRC Press, 1991;81-99.
16. Nikulin M, Pasanen AL, Berg S, Hintikka EL. Stachybotrys atra growth and toxin production in some building materials and fodder under different relative humidities. Appl Environ Microbiol 60:3421-3424 (1994).
17. Johanning E, Gareis M, Yang CS, Hintikka EL, Nikulin M, Jarvis B, Dietrich R. Toxicity screening of fungal (Stachybotrys chartarum) field samples and indoor exposure. Mycotoxin Res 14:60-73 (1998).
18. Dillon HK, Heinsohn PA, Miller JD (eds). Field Guide for the Determination of Biological Contaminants in Environmental Samples. AIHA Biosafety Committee. Fairfax, VA:American Industrial Hygiene Association, 1996.
19. Hanelt M, Gareis M, Kollarczik B. Cytotoxicity of mycotoxins evaluated by the MTT-cell culture assay. Mycopathologica 128:167-174 (1994).
20. Gareis ML. Cytotoxicity testing of samples originating from buildings. In: Fungi and Bacteria in Indoor Air Environments (Johanning E, Yang CS, eds). Proceedings of the International Conference, 6-7 October 1994, Saratoga Springs, New York. Albany, NY:Eastern New York Occupational Health Program, 1995;139-145.
21. Rosenstreich DL, Eggleston P, Kattan M, Baker D, Slavin RG, Gergen P, Mitchell H, McNiff-Mortimer K, Lynn H, Ownby D, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma [see comments] N Engl J Med 336(19):1356-1363 (1997).
22. Peat JK, Dickerson J, Li J. Effects of damp and mould in the home on respiratory health: a review of the literature. Allergy 58:120-128 (1998).
23. Dales R, Miller D, White J, Dulberg C, Lazarovitz AI. Influence of residential fungal contamination on peripheral blood lymphocyte population in children. Arch Environ Health 53 (3):190-195 (1998).
24. Polgar C, Promadhat V. Pulmonary Function Testing in Children: Techniques and Standards. Philadelphia:W.B. Saunders, 1971;100-153.
25. Knudson RJ, Slatin R, Lebowitz M, Burrows B. The maximal expiratory flow-volume curve. Normal standards, variability, and effects of age. Am Rev Respir Dis 113:557-600 (1976).
26. Knudson RJ, Lebowitz M, Holberg CJE, Burrows B. Changes in the normal maximal expiratory row-volume curve with aging. Am Rev Respir Dis 127:725-734 (1983).
Abstract
This is a review of exposure conditions, clinical presentation, and
morbidity of children and adults with indoor fungal exposure such as toxic
Stachybotrys chartarum. Indoor exposure was characterized using
different methods including microscopic, culture, cytotoxicity screening
tests, and chemical analyses. Clinical case histories and physical and
laboratory findings are presented of children (age < 18 years, n =
22; mean age 9 years; 60% females) and adults (age >18 years, n =
125; mean age 39 years, 67% females) who consulted an environmental health
specialty clinic. In the pediatric patients' exposure history, widespread
fungal contamination of water-damaged building materials with known toxic or
allergic fungi was identified. Primarily disorders of the respiratory
system, skin, mucous membranes, and central nervous system were reported.
Some enumeration and functional laboratory abnormalities, mainly of the
lymphatic blood cells, were observed, although no statistically significant
differences were found. IgE or IgG fungi-specific antibodies, used as
exposure markers, were positive in less than 25% of all tested cases. In an
evaluation of a symptomatic girl 11 years of age (sentinel case
investigation) living in an apartment with verified toxigenic fungi (i.e.,
S. chartarum), several health indicators showed improvement after
exposure cessation. Key words: allergy, bioaerosol, exposure, fungi,
health, morbidity, mycotoxins, Stachybotrys, toxicity. -- Environ
Health Perspect 107(suppl 3):489-494 (1999).
http://ehpnet1.niehs.nih.gov/docs/1999/suppl-3/489-494johanning/abstract.html