|
ORBITAL APEX
SYNDROME DUE TO ASPERGILLOSIS
Case report Yvens B. Fernandes1, Ricardo Ramina1, Guilherme Borges2, Luciano S.Queiroz3, Marcos V.C. Maldaun4, Jayme A. Maciel Jr.5
Orbital apex syndrome is a paralysis of all three nerves supplying the external ocular muscles and a sensory deficit in the distribution of the first division of the trigeminal nerve, combined with an optic nerve lesion1. Aspergillus is a fungus found in soil and organic debris. It commonly presents as a localized disease of the lungs or paranasal sinuses and mainly affects immunocompromised individuals, usually as a fatal opportunistic infection in acquired immunodeficiency syndrome (AIDS)2,3. Patients with diabetes, leukemia and lymphoma are at higher risk. It can also affect normal or mildly immunocompromised patients, usually as an invasive chronic form4. Opportunistic infections frequently involve the anterior and posterior segments of the eye, orbit and sinuses, with possible secondary intracranial extension. Orbital aspergillosis is a rare condition that may clinically mimic non-specific orbital inflammatory disease. We report on a case of Aspergillus fumigatus infection, which caused an orbital apex syndrome and later a temporal brain abscess in a non-immunocompromised patient.
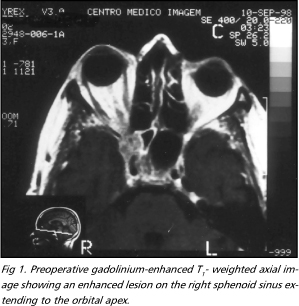
CASE A 73-year-old Caucasian woman presented with a one-year history of headaches. She also complained of facial numbness and pain in the first trigeminal division territory in the last four months, ptosis, diplopia and visual blurring on the right side. Neurological examination disclosed complete right-sided ophthalmoplegia with mydriasis, first trigeminal division hypoalgesia, diminished corneal reflex and severe visual loss. Magnetic resonance imaging (MRI) showed an enhanced lesion on the right sphenoid sinus extending to the orbital apex. Human immunodeficiency virus (HIV) tests to point out AIDS were negative. Blood tests revealed she was immunocompetent.
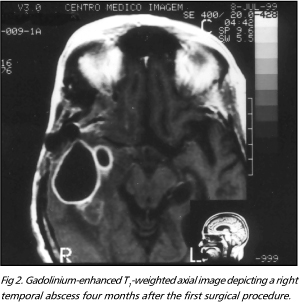
In view of the examination results an orbital apex syndrome was considered. The presumptive diagnosis was a skull base tumor. A right pterional craniotomy was performed with opening of the orbital apex. An infiltrative process involving the orbital fat, vessels and nerves was found. Neurolysis of the first and second branches of the trigeminal nerve up to Meckel's cave was carried out. The postoperative course was uneventful, the patient was relieved of her trigeminal pain. Histological examination showed cellular contents compatible with "chronic active inflammatory process". Based on this diagnosis oral prednisone (40 mg/day) was prescribed and she was discharged five days after the surgical procedure. Four months later the patient presented episodes of low fever, loss of appetite and lately mental confusion. A new MRI revealed a large lesion pointing out to a right temporal abscess. She was immediately submitted to surgical drainage. Microscopic examination of the exudate displayed numerous hyphae of Aspergillus fumigatus. Amphotericin B (1.0 mg/kg/day) was given by intravenous infusion, during three weeks. After three weeks a control CT scan still showed residual abscess and a new drainage of the abscess was done. The patient was discharged after two months of maximum recommended doses of antimycotic therapy (1.2 mg/kg/day).
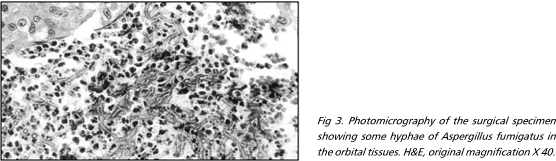
One month later she developed again signs of systemic infection and the CT scan showed a persistent large right temporal abscess. A new surgical procedure was carried out with total removal of the abscess capsule and removal of the bone flap. The patient was kept under amphotericin B given intravenously but died two months later due to respiratory and renal failure. Unfortunately a review of a second section of the histogical specimen of the first surgery showed a few hyphae morphologically compatible with Aspergillus sp. In spite of the high gravity of human aspergillosis and its dissemination, in this case, the misdiagnosed histological examination during the first admission undoubtedly contributed to the fatal outcome of our patient.
DISCUSSION The orbital apex syndrome might have other causes like optic nerve glioma, infraclinoid aneurysm of the internal carotid artery, trauma, orbital tumors and Paget's disease. Only rarely is aspergillosis the causative pathology1,5. Aspergilli are moulds with a ubiquitous distribution in indoor and outdoors environments. In humans, almost all the invasive Aspergillus infections are caused by Aspergillus fumigatus. It was first described by Fresenius in 1863, who isolated it from an airway infection in poultry6. In invasive human infections A. flavus, A. glaucus, A. niger, A. restrictus, A. terreus and A. versicolor have been found as causative agents, although they are rare and of minor medical importance. Aspergillus fumigatus is the most frequent species isolated in human infections, followed by A. flavus4,7. Invasive aspergillosis is an opportunistic infection and occurs very often in the granulocytopenic patient. Predisposing causes include alcoholism, low-dose prednisone therapy and insulin-dependent diabetes mellitus. The route of infection is frequently by inhalation of Aspergillus spores and conidia or airborne metabolites of Aspergillus, causing at first allergic aspergillosis. Acute bronchopulmonary aspergillosis is increasingly being observed. Peribronchial eosinophilic infiltrations may occur and the disease can lead to exogenic allergic alveolitis, the so-called "farmer's lung". Acute allergic conjunctivitis and rhinitis have been reported. Most allergic diseases caused by Aspergillus species are attributable to A. fumigatus6. The main routes of central nervous system (CNS) contamination are hematogenous dissemination from a distant primary source, mainly lung, and contiguous spread from an adjacent focus such as orbit or paranasal sinuses3,8,9. Involvement of the CNS is present in 10-15% of patients with disseminated disease4. It may manifest as single solid granuloma, multiple abscesses, necrotic lesions or meningitis10. Recently Coleman et al.10 made a detailed review of the literature and showed that invasive CNS aspergillosis is a dramatic disease, mainly in the immunosuppressed host, with mortality rate over 90% in most series. The definitive diagnosis of invasive aspergillosis is often confirmed post-mortem, especially in the immunocompromised host3. Invasive infections can be detected by imaging procedures such as X-ray, CT scan, MRI and sonography, but laboratory confirmation is of great importance. Respiratory secretions, bronchoalveolar lavage fluid as well as other clinical specimens from infected sites should be examined both under the microscope and in cultures. Some problems can arise with immunological procedures in the diagnosis of aspergillosis. Patients with allergic aspergillosis often show high specific IgG antibody titers against Aspergillus polysaccharide and/or glycoprotein antigens combined with high serum IgE titers and also often specific anti-Aspergillus IgA titers3. On average, about 90% of the patients with aspergillomata show specific IgG antibody titers against Aspergillus antigens, often combined with specific IgA titers. Altogether, the interpretation of serological results in Aspergillus-associated diseases is problematic and must be combined with clinical diagnostic procedures, and microscopic and microbiological techniques3,6. Allergic diseases are generally treated symptomatically and the causative allergen must be eliminated as far as possible. Systemic aspergillosis is a life threatening opportunistic infection that requires specific antimycotic therapy. In some cases, antimycotic therapy is able to stop the infection but has no curative effect until the patient's underlying state of immunosuppression has improved. Despite its high nephrotoxicity, amphotericin B is the first-line drug for systemic therapy. In the case of aspergillomata treatment includes aggressive surgical debridement and antifungal therapy with amphotericin B, itraconazole, voriconazole or intracavitary drug administration2,5,11-14. Despite these efforts mortality remains very high3,6. We reported a rare case of invasive fungal aspergillosis of the CNS, in a 73-year-old immunocompetent female, causing orbital apex syndrome and later a temporal brain abscess; she died ten months later due to respiratory and renal failure in spite of antifungical treatment.
REFERENCES 1. Bray WH, Giangiacomo
J, Ide CH. Orbital apex syndrome. Surv Ophthalmol 1987;32:136-140. 2. Weinstein JM, Sattler FA, Towfighi J, Sassani J, Page RB. Optic neuropathy and paratrigeminal syndrome due to Aspergillus fumigatus. Ach Neurol 1982;39:582-585. 3. Denning DW. Invasive
aspergillosis. Clin Infect Dis 1998;26:781-805. 4. Swift AC, Denning DW.
Skull base osteitis following fungal sinusitis. J Laryngol Otol
1998;112:92-97. 5. Massry GG, Hornblass
A, Harrison W. Itraconazole in the treatment of orbital aspergillosis.
Ophthalmology 1996;103:1467-1470. 6. Latgé JP.
Aspergillus fumigatus and aspergillosis. Clin Microbiol Rev
1999;12:310-350. 7. Murai H, Kira J,
Kobayashi T, Goto I, Inoue H, Hasuo K. Hypertrophic cranial
pachymeningitis due to Aspergillus flavus. Clin Neurol Neurosurg
1992;94:247-250. 8. Wiles CM, Kocen RS, Symon L, Scaravilli F. Aspergillus granunola of the trigeminal ganglion. J Neurol Neurosurg Psychiatry;1981,44:451-455. 9. Camarata PJ, Dunn
DL, Farney AC, Parker RG, Seljeskog EL. Continual intracavitary
administration of amphotericin B as an adjunct in the treatment of
aspergillus brain abscess: case report and review of the literature.
Neurosurgery 1992;31:575-579. 10. Coleman JC, Hogg GG,
Rosenfeld JV, Waters KD. Invasive central nervous system aspergillosis:
cure with liposomal amphotericin B, itraconazole, and radical surgery:
case report and review of the literature. Neurosurgery 1995;36:858-863.
11. Scamoni C, Dario A, Pozzi M, Dorizzi A. Drainage of aspergillus "primitive" brain abscess with long-term survival. J Neurosurg Sci 1990;32:155-158. 12. Cahill KV, Hogan
CD, Koletar SL, Gersman M. Intraorbital injection of amphotericin B for
palliative treatment of Aspergillus orbital abscess. Ophthal Plast
Reconstr Surg 1994;10:276-277. 13. Borges-Neto V, Medeiros S, Ziomkowski S, Machado A. Successful treatment of mucormycosis and Aspergillus sp, rhinosinusitis in an immunocompromised patient. BJID 1998;2:209-211. 14. Schwartz S, Milatovic D, Thiel E. Successful treatment of cerebral aspergillosis with a novel triazole (voriconazole) in a patient with acute leukaemia. B J Haematol 1997;97:663-665. Disciplina de Neurocirurgia (DNC) e Disciplina de Neurologia Clínica (DNE) do Departamento Neurologia e Departamento de Anatomia Patológica (DAP) da Faculdade de Ciências Médicas da Universidade Estadual de Campinas (UNICAMP), Campinas SP, Brasil : Médico Contratado, DNC; Professor Doutor, DNC; Professor Doutor, DAP; Médico Residente, DNC; Professor Associado, DNE. Received 1 December 2000, received in final form 23 May 2001. Accepted 28 May 2001. Dr. Yvens Barbosa Fernandes - Rua Maestro João de Túlio 140 / 82 - 13024-160 Campinas SP - Brasil. E-mail: yvens@uol.com.br |